Kennedy v. Braidwood: The SCOTUS Case that Could Gut Preventive Care
A conversation with Natalie Davis, CEO of United States of Care
Quick poll: Who’s heard of Kennedy v. Braidwood?
No? You’re not alone. Despite its enormous implications, this Supreme Court case has flown largely under the radar — even among those of us who follow healthcare closely.
But, the stakes couldn’t be higher. Kennedy v. Braidwood could quietly dismantle one of the core tenets of the Affordable Care Act: the requirement that insurers cover preventive services at no cost.
As is often the case in healthcare, women have the most to lose.
If the Court strikes down the preventive care mandate, access to critical screenings and other preventive services — from well-woman visits to mammograms and colonoscopies — would be at risk for 151 million Americans who rely on employer-sponsored insurance. The result? A patchwork system, much like what we’ve seen with abortion post-Roe, where access to preventive care depends on where you live or who you work for.
This fight isn’t new. The Trump administration tried and failed to repeal the ACA in its first term, but legal attacks on its core provisions have persisted. Now, with this case reaching the Supreme Court, the threat to no-cost preventive care is more real — and urgent — than ever.
That’s why I sat down with Natalie Davis, CEO of United States of Care, to unpack what’s at stake. From the future of maternity care to Medicaid to SCOTUS rulings, Natalie is my first call when I need to understand what’s really happening behind policy headlines.
For some quick background, United States of Care is a nonpartisan policy organization working to ensure that everyone in the U.S. has access to quality, affordable healthcare no matter their income, background, or ZIP code. What I admire most about their work is that it starts with listening: to everyday people, to “kitchen table” concerns, and to what really matters when it comes to healthcare. They work across the aisle and the public and private sectors to push for policies rooted in what real people actually want from our healthcare system: affordability, access, and simplicity.
In our conversation below, Natalie breaks down the nuts and bolts of this SCOTUS case, why it’s different from past ACA challenges, and what we can do about it.
What’s at Stake (and Who’s Behind It)
Carolyn Witte (CW): Let’s start with the basics — what is Kennedy v. Braidwood, and why should people care?
Natalie Davis (ND): Kennedy v. Braidwood (formerly Braidwood v. Becerra) challenges a key provision of the Affordable Care Act: the requirement that private insurers cover a broad range of preventive services without any out-of-pocket costs to patients (think: co-pays, deductibles, or coinsurance).
Right now, 151 million people with employer-sponsored insurance have access to no-cost (aka “free”) cancer screenings, maternal health services, HIV prevention medications (PrEP), and more. The plaintiffs argue that the entity responsible for recommending these preventive services — the U.S. Preventive Services Task Force — wasn’t constitutionally appointed because its members weren’t confirmed by the Senate. This seemingly procedural attack is actually a backdoor effort to dismantle no-cost preventive care.
If the Supreme Court rules against the preventive services mandate, private insurers and employers would no longer be required to cover these services. This means that 151 million people — including 37 million children — could face new out-of-pocket costs for routine screenings and essential care proven to help get and keep Americans healthy.
CW: There have been attempts to repeal and undermine the Affordable Care Act in the past. How is this attack different? Who is driving it?
ND: Unlike previous attacks that aimed to repeal the ACA entirely, Braidwood takes a targeted aim at employer-sponsored insurance — the backbone of healthcare for more than half of the country — and specifically, the no-cost preventive services Americans have come to rely on for over a decade.
This case has been brewing for some time. It was first filed in Texas in 2020 by a group of plaintiffs, including Dr. Steven Hotze, a Christian activist and founder of Hotze Health & Wellness Center. They argue that covering certain preventive services — particularly, PrEP, the HIV prevention medication — violates their religious beliefs. In addition to religious objections, the case also claims that the U.S. Preventive Services Task Force — the body that recommends which services must be covered — is unconstitutional because its members weren’t confirmed by the Senate.
In 2023, Judge Reed O’Connor (known for previous rulings against the ACA) sided with the plaintiffs, striking down the no-cost preventive care mandate for services recommended by the Task Force. The Biden administration appealed, and now, the case is in the hands of the Supreme Court with a ruling expected in June.
Zooming out, this case is about more than employer choice and procedural technicalities. If these protections are rolled back, 151 million Americans could be left to navigate a fragmented system where access to basic, evidence-based preventive care integral to individual and public health depends entirely on your employer.
Why Women (and Everyone) Should Care About This
CW: The scale of the potential impact here is striking. How does this case specifically impact women’s health?
ND: As you well know, women rely on preventive care at higher rates than men, which means they have the most to lose if this provision is struck down. The services specifically at risk include:
Mammograms and breast cancer screenings
Cervical cancer screenings (Pap smears and HPV testing)
Gestational diabetes screening
Pre-eclampsia prevention (e.g. aspirin therapy)
Prenatal and postpartum care
Contraceptive counseling and services
Maternal mental health screenings
To be clear, this ruling wouldn’t outlaw these services; instead it could shift the cost to patients by removing the requirement that employer sponsored insurance plans cover them 100%.
CW: What do we know about the importance of no-cost coverage for preventive care? Does usage really decline when there’s patient responsibility?
ND: The short answer is yes, usage is likely to decline. There’s extensive research showing that when cost-sharing is introduced, people are significantly less likely to use preventive care, leading to delayed diagnoses, worsened health outcomes, and higher overall healthcare costs.
We hear the same thing in our listening work with Americans around the country — specifically that cost is the number one source of anxiety when seeking care. Even small out-of-pocket expenses deter people from getting preventive screenings, especially among low-income Americans.
To put some hard numbers behind this, since no-cost cancer screenings became available, cancer deaths have declined by 17%. Modern mammography programs have reduced breast cancer mortality by over 40% and Pap smears have led to a decrease of over 50% of cervical cancer incidence and mortality. All of these gains are at risk if we reintroduce cost-sharing.
Fighting Back: What We Can Do To Protect Preventive Care
CW: What about state-level protections? Could states step in to require insurers to cover preventive services at no cost?
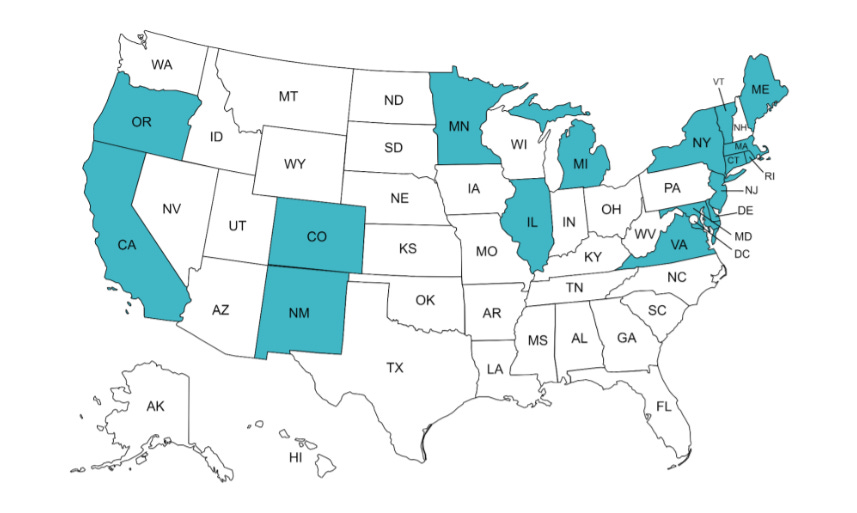
ND: Yes, states have a major role to play here and preemptively as we await a final ruling. United States of Care has been partnering with states across the nation to pass legislation to protect access to preventive services for as many people as possible. Since the case was filed, 17 states have enacted laws requiring insurers to maintain these protections.
But ultimately, state action can only go so far in terms of protections. The responsibility rests with the Supreme Court to correct this ruling and protect access to these services for everyone, no matter what state you live in or who you work for.
CW: If this provision is struck down, what can people do?
Call your employer and state legislators – Let them know that access to free preventive care matters to you — and demand they take action to protect it.
Keep an eye on your insurance coverage. If you notice changes to what’s covered, speak up and push back.
Support organizations like United States of Care – They are actively working to ensure state-level protections. Donations of any size can help support their work.
CW: RFK Jr. and the Make America Healthy Again (MAHA) movement emphasize health and chronic disease prevention, but Kennedy v. Braidwood threatens to gut one of the most effective tools we have for preventing and managing chronic conditions. How do you make sense of this? What should we be watching for in terms of the administration's response?
ND: If we’re serious about preventing chronic disease, we have to ensure people can access preventive care, full stop. Services like cancer screenings, blood pressure checks, diabetes testing, and mental health screenings are foundational to making people healthy and catching conditions early.
That’s why it was noteworthy that the Trump administration recently submitted a brief signaling support for continuing the defense of the ACA’s preventive services mandate. This bipartisan continuity is incredibly encouraging — and a recognition that these protections are not just popular across the aisle, but essential. Moreover, it shows they might recognize the potential contradiction here and how turning back the clock on preventive care could decimate MAHA’s efforts.
With oral arguments happening in front of the Supreme Court soon, it’s important that the administration champion the value in these services as a cornerstone of a healthcare system that aims to get and keep people healthy.
CW: Final thoughts — what’s your biggest concern, and what gives you hope?
ND: My biggest concern is that people don’t realize what’s at stake — that Kennedy v. Braidwood gets lost in the noise of political upheaval and the fatigue so many people feel right now. I am hopeful that through more conversations like these that put this case on people’s radars, we can spread awareness and drive action.
Zooming out further, I am hopeful, too, that employers, insurers, and policymakers can still choose to do the right thing, regardless of how SCOTUS rules in June. Even if these protections are no longer required by federal law, they can recognize the proven value of preventive care and commit to preserving it at no-cost to patients — because it’s the right thing to do.
If this breakdown lit a fire in you like it did for me, here are a few ways to dive deeper:
Learn More: Explore the United States of Care Preventive Services Hub for resources, FAQs, and updates on the case.
Track State-Level Protections: Use the KFF State Health Policy Dashboard to see what your state is doing to protect no-cost preventive care.
Advocate: Call your state representative and ask what they’re doing to preserve preventive service protections — and let them know this matters to you.
P.S…
I’d be remiss not to mention the deeper issue underlying all of this that kept bubbling up for me in my conversation with Natalie: the fact that healthcare in America is tied to your employer in the first place. This system — a byproduct of post-WWII wage controls and tax policy — is the root cause of so many misaligned incentives in our healthcare system from employers shouldering gargantuan healthcare costs they can’t control to people losing coverage when they leave their job to what Kennedy v. Braidwood proposes: preventive care as optional rather than essential.
To be clear: I’m 1000% in favor of working within the current guardrails to protect access to preventive care through employer-sponsored care — this is the de facto way half of the country currently gets healthcare. But it’s hard to ignore the root-cause diagnosis here: the fragility of a system where your access to basic healthcare depends on where you work.
As someone who ran a company that provided health insurance and benefits for 400+ employees, I can tell you that deciding what to cover and not cover at the individual service level is an absolute nightmare for an employer. This is the standard for “non-required” services like fertility and mental health; the possibility of this cascading further to preventive care is terrifying. It’s not just bad for employees; it’s bad for business — it’s distracting, costly, and complex. And frankly, 90%+ of employers have no interest in making those decisions let alone the expertise to do so thoughtfully.
So the question is: how do we undo this? Can we build a new bridge while we patch up the old one? If you’re thinking about this too — let’s talk. I’d love to hear from you.






Corrupt MAGA Rich-owned SCOTUS. … no longer respected by citizens